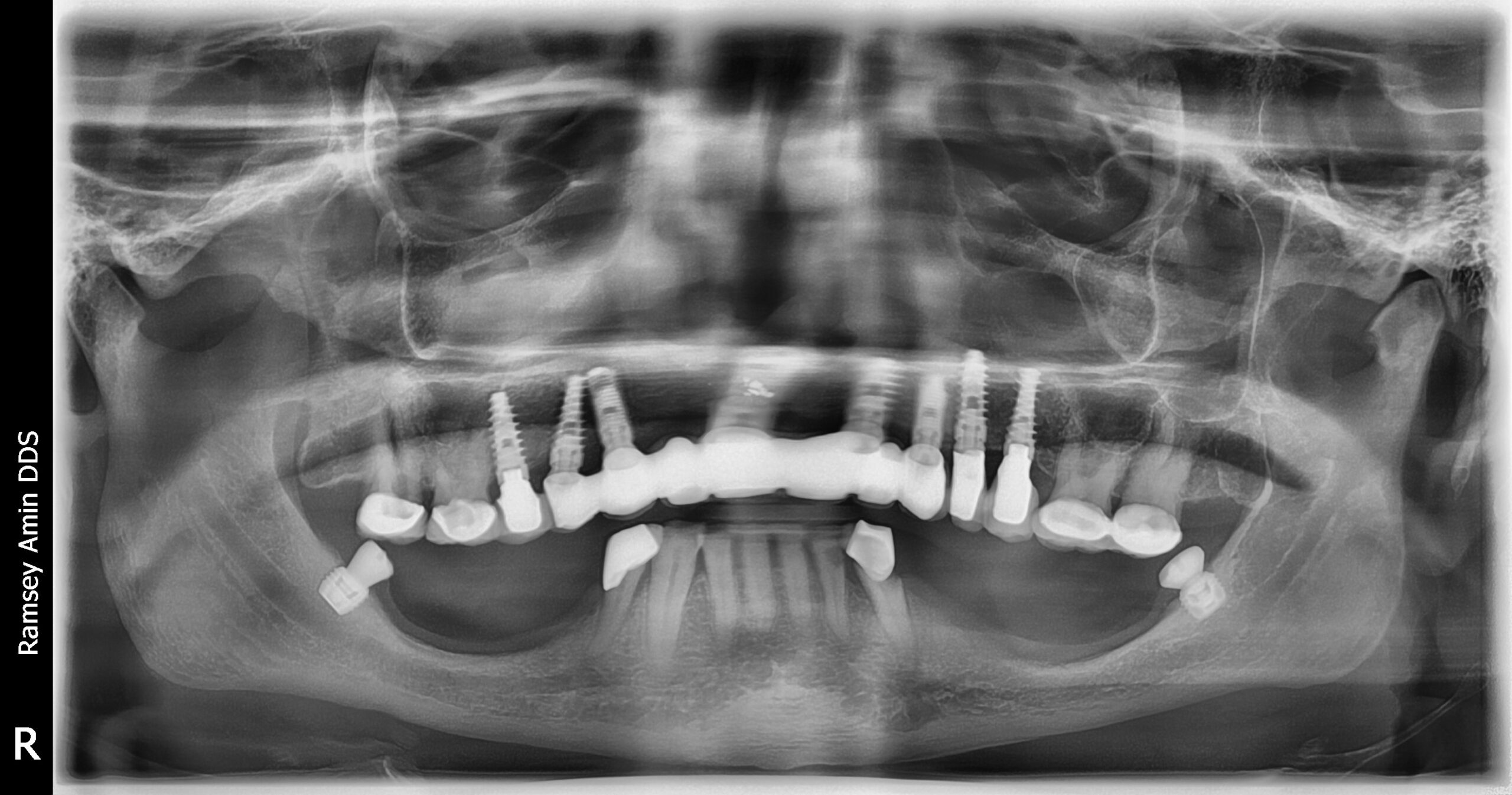
The topic I want to talk about today (regarding full mouth implants) is something I’m seeing more and more often—patients who already have several dental implants but are now losing additional teeth. This is especially common in the baby boomer age group.
So, when do we stop adding implants and instead consider converting to a full-arch bridge using the implants you already have? That’s what I want to dive into.
Let’s say, over the years, you’ve had one, two, or three implants placed—maybe one here, another there, and so on. On top of that, you might already have four or five implants in your mouth, but are now losing a couple more teeth. This happens often as we age because of root decay. Root decay is common when our roots become exposed—those areas aren’t protected by enamel like the rest of the tooth and can develop cavities in places you can’t even see.
This is something I’m encountering more frequently, especially with my complex cases. Many of my patients come to me because no one else wants to or can treat them—it’s just too complicated.
But here’s the thing: if you already have four, five, or six implants in the right distribution (say, one here, one there, spaced evenly), those implants can often support an entire bridge.
Here’s a key point: more implants aren’t always better.
What’s better is having enough bone and enough space between the implants. Crowded implants—especially in the front of the mouth where bone has less blood supply—can lead to bone loss. So if you already have four, five, or six well-placed implants, it might be worth considering converting them into a full-arch restoration instead of just adding more.
Repurposing Existing Implants
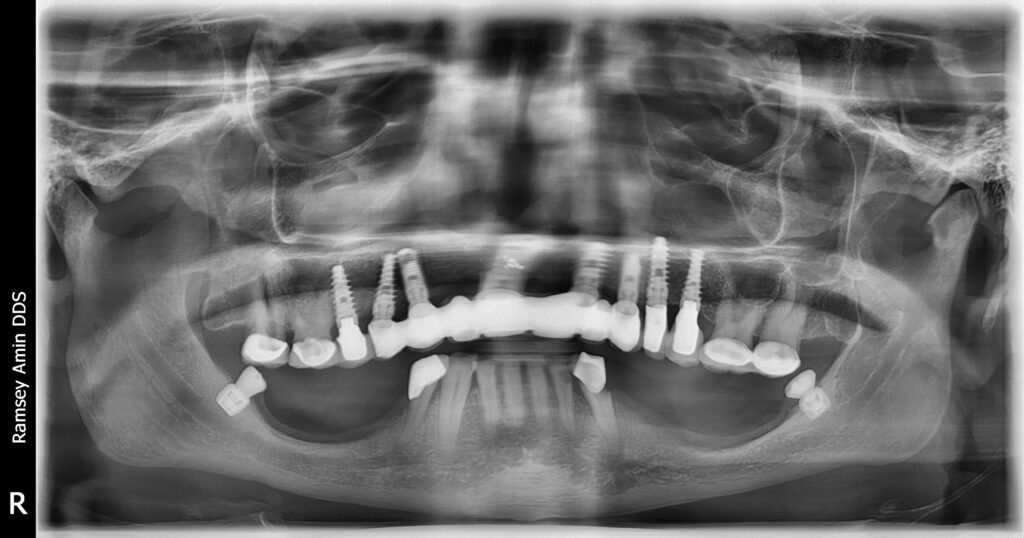
Repurposing your existing implants for a full-arch bridge isn’t as simple as taking off a crown and putting on a new bridge—it’s more complicated than that. For example:
- You might have implants from different manufacturers in your mouth (think of it like having a Honda here, a Toyota there, and maybe even a Mercedes). Getting everything to work together can be tricky.
- Sometimes we don’t even know what type of implant was used because records aren’t available or the previous dentist isn’t around anymore.
- Implants might be too close together or not placed deep enough for full-arch support.
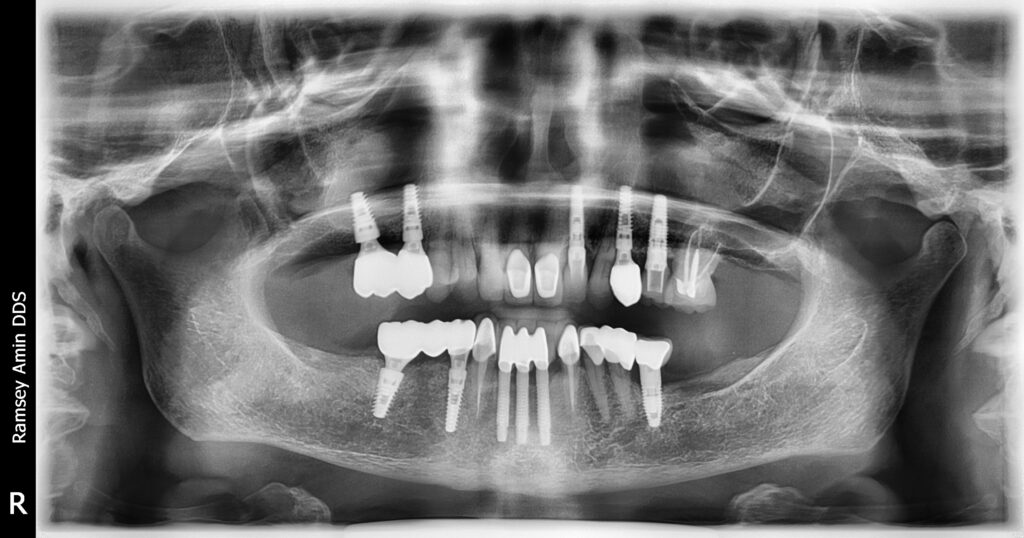
The goal with these cases is to create a strong horseshoe-shaped bridge (like an All-on-4 or All-on-6). But if the implants aren’t deep enough or properly aligned with each other, it can weaken the bridge and lead to issues like uneven smiles or poor aesthetics.

Transition Line and Smile Design
Another factor to consider is something called the “transition line.” This refers to how much gum tissue shows when you smile.
If we need to add pink material (to mimic gum tissue) as part of the restoration, we have to ensure it looks natural when you smile. The implants also need to be level with each other—if one is too high or too low compared to the others, it can throw off your smile line.
Why Not Just Add More Implants?
It might seem like adding another implant is easier or cheaper than converting to a full arch (or full mouth implants) — but that’s not always true. In fact:
- The cost of these cases often comes from creating the prosthetics (the teeth), which can be more expensive than surgery.
- It takes a high level of skill and expertise to make these restorations strong enough not to break and aesthetically pleasing so they look natural.
- Sometimes we even have to remove existing implants if they’re not usable due to bone loss or poor placement.
- Crowding more implants in the front very often results in bone loss!
For example, if an implant has already lost a third or half of its supporting bone, it’s not worth keeping it in place—it’ll only cause problems down the road.
Making Implants Work Together
One way we can make different types of implants work together is by using multi-unit abutments. These are universal connections that allow us to scan and fabricate restorations more easily. Think of it like having a Phillips head screwdriver—it works universally across many screws. Multi-unit abutments also make it easier for another dentist to work on your case in the future if needed.
But keep in mind: most dental implant systems are proprietary. One manufacturer’s screw won’t work with another manufacturer’s implant. That’s why treating cases with multiple types of implants requires experience and access to a wide inventory of parts.
The Risks of Too Many Implants
I recently saw a patient who had way too many implants on both their upper and lower jaws. By the time we removed everything that wasn’t salvageable, there was almost no bone left. Now I’m forced to place zygomatic implants (which anchor into the cheekbone) because all the upper jawbone is gone. This could’ve been avoided with fewer, better-spaced implants from the start.
Less is often more when it comes to implants—it allows for proper cleaning (with tools like Waterpiks or proxy brushes) and ensures long-term success.
The Importance of Expertise
Lastly, having an expert lab partner cannot be underestimated. While some dental offices handle these cases entirely in-house—and I respect that approach—there’s no substitute for working with an experienced lab technician who understands how to create durable, beautiful restorations.
The last thing you want is to spend time and money redoing something because it wasn’t done right the first time.
If you’re reading this post, chances are you’ve already been through some ups and downs with dental implants (full mouth implants, multiple implants or single implants) —you’ve lost some bone, replaced it, and maybe even lost faith in the process at times.
But trust me: with proper planning and execution by someone experienced in these complex cases, there’s hope for achieving a long-lasting solution that looks great and functions well.