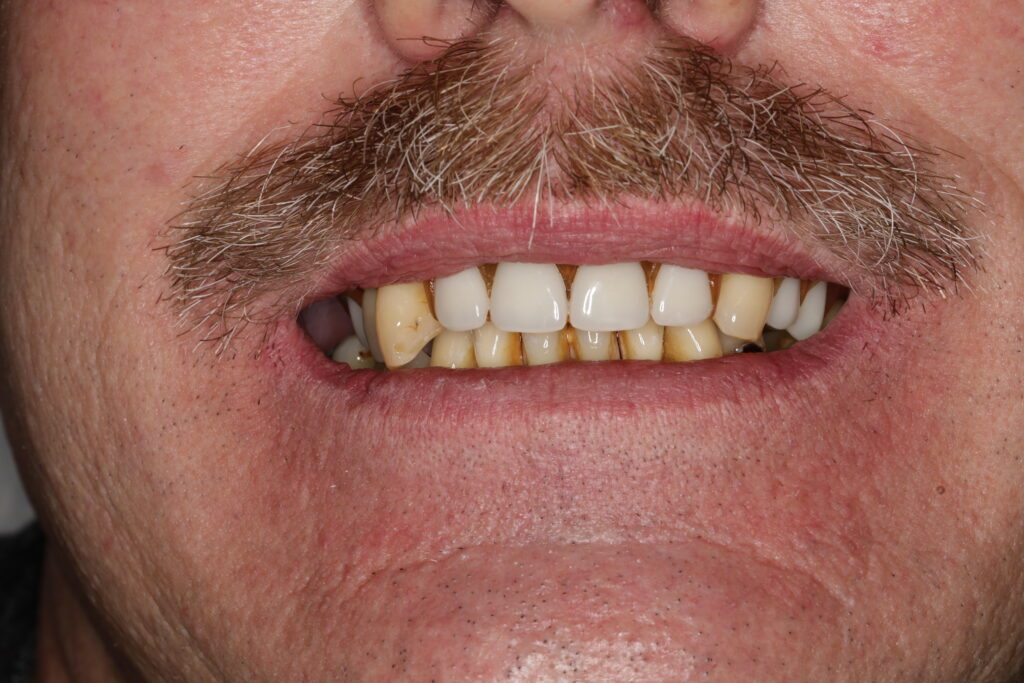
A patient might walk into my office with what I call a “terminal dentition” case. In this situation, all teeth need to be extracted for full mouth implants. Saving the teeth would not be a practical option. Recently, I treated a man facing this exact scenario, dealing with multiple oral health issues:
- Severe gum disease
- Bite collapse due to missing teeth and advanced gum disease infection
- Decay of numerous teeth
Fortunately, there was no teeth grinding (bruxism), which often compounds gum disease and bite collapse. The plan was full mouth extraction and full mouth dental implants.






Pre-Treatment Preparation
Before diving into treatment in a terminal teeth case, I always prioritize the patient’s overall health. In cases of severe gum disease, I advise checking for other conditions. This is especially important when a patient hasn’t seen a doctor recently. Testing for conditions like diabetes can help, as they impact oral and implant health.
After ensuring he was medically optimized, including appropriate blood pressure and diabetes management, I moved forward with creating records.
Treatment Planning
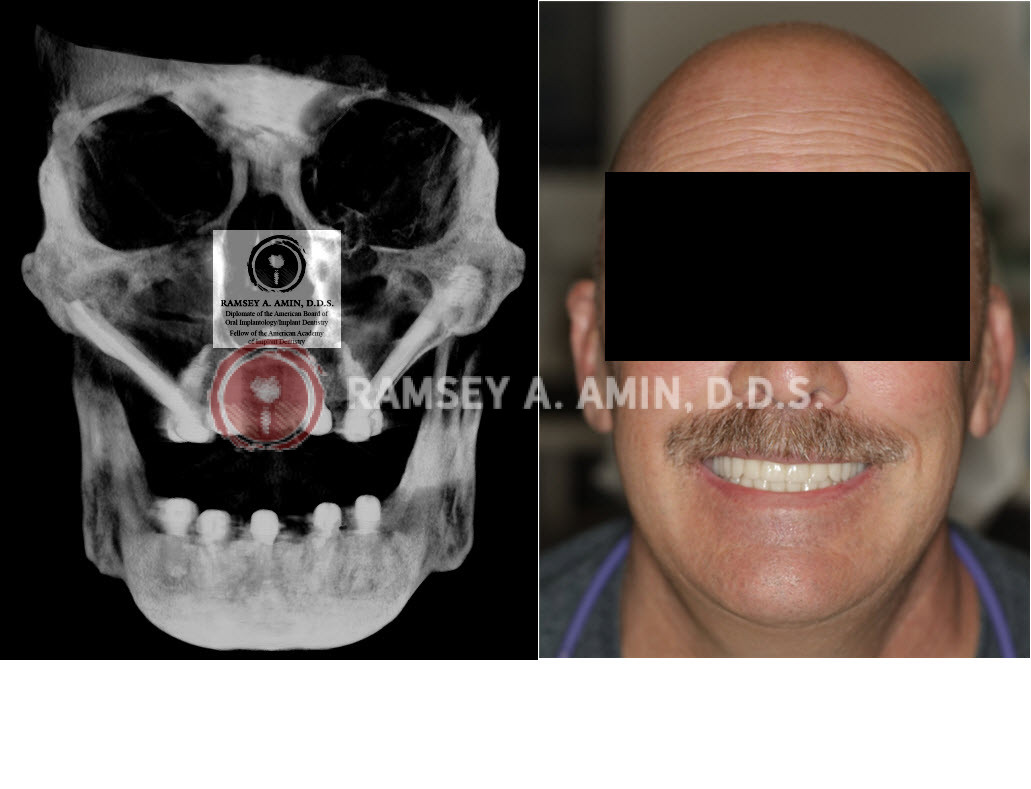
The collapsed bite required opening his vertical dimension to recreate his former bite. My goal was to design teeth that not only fit his mouth better but also enhance his smile. Looking at his “before” picture, it was clear his teeth didn’t suit his face, likely causing him to hide his smile.
I used cutting-edge technology for treatment planning:
- Digital scanning molds
- Face scans
- Pre-surgical teeth design
The Surgical Process
On surgery day, I:
- Extracted all remaining teeth
- Placed all implants simultaneously
- Performed the procedure under IV sedation in my sterile surgical suite
- Used a photogrammetry scanner to record implant positions
For pain management, I administered Exparel, keeping him numb for about 3 days. This approach allowed me to avoid stronger opioid painkillers like Vicodin or Percocet, relying instead on ibuprofen. I also incorporated PRP and PRF made from his blood to enhance healing.
Immediate Results
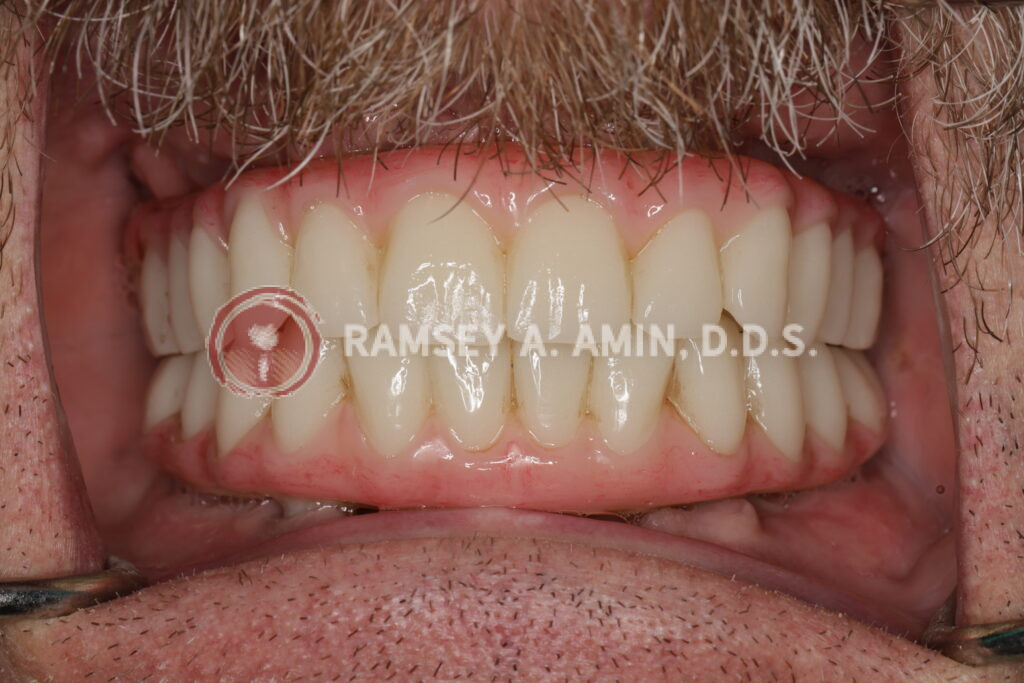
The day after surgery, I fitted him with pre-surgically designed PMMA healing teeth. The transformation was remarkable – he had a perfect bite, and all signs of disease were gone. While some swelling and bruising occurred, these were short-lived. Within days, he was smiling and adapting to his new bite.
Implant Details
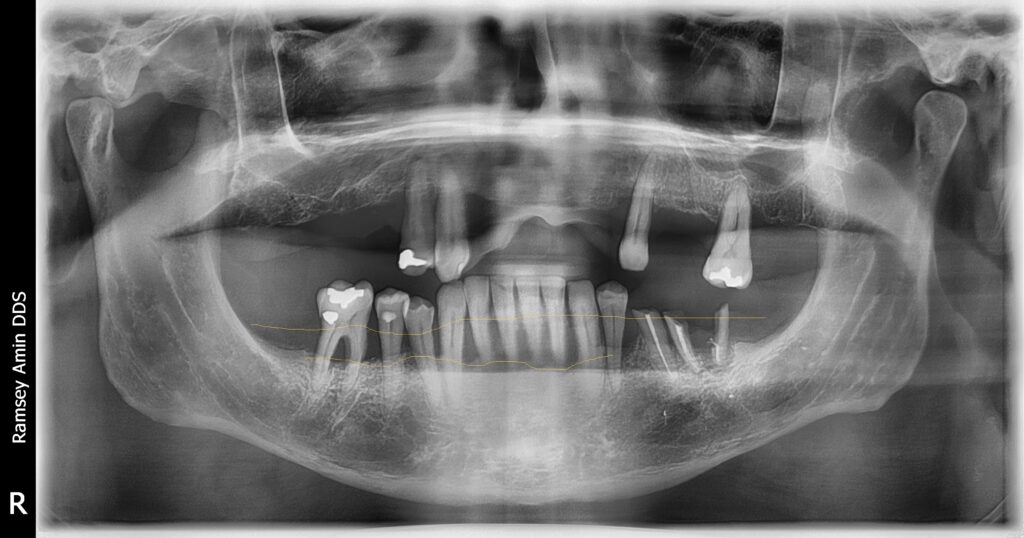
After all teeth were removed, the patient received:
This configuration eliminated any cantilever. Both the healing teeth and the final zirconia prosthesis were made on multiunit abutments. This allows for an excellent fit and long-term hygiene access.









A Note on Dental Cantilevers
A dental cantilever is a part of a dental prosthesis that extends beyond the last supporting implant or tooth. While sometimes necessary, excessive cantilevers can lead to complications like implant failure or prosthesis fracture, especially in the upper jaw. By using zygomatic and pterygoid implants, I was able to avoid these potential issues for this patient.
I would highly suggest you read this post on All-on-4 Complications

Upper Jaw Considerations
For the upper jaw, which was very hollow with little bone density, I used zygomatic and pterygoid dental implants. This approach is superior to sinus bone grafting, using small implants, or crowding a standard all-on-4 with a cantilever, which could lead to fractures or failures.
Patient Satisfaction When All Teeth Need to be Extracted
The patient was thrilled with the results (even though all teeth needed to be extracted) and even made a video sharing his experience with the process.
I take great pride in providing this level of care, which few dental practices nationwide can match. It’s a testament to my commitment to patient safety and long-term dental implant solutions.