One of the long-term risks associated with dental implants is a condition called Peri-implantitis.
Peri-implantitis Definition: Infectious disease that causes inflammation of the surrounding gum and bone of an already integrated dental implant, leading to the loss of supporting bone.
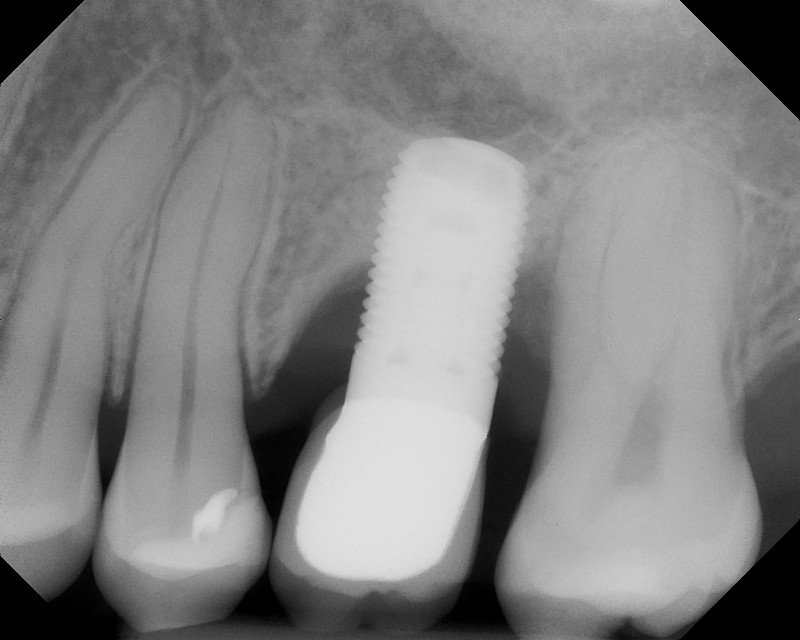
These two x-rays show implants with bone loss.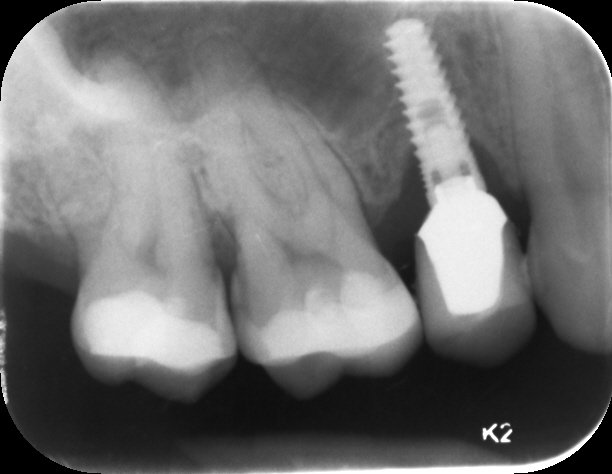
Bone Loss Around Dental Implants
Bone, for a variety of reasons, is lost around the dental implant. This condition generally occurs without the patient being aware of it. There are many factors on why this can happen. Some dental implants on some patients will develop bone loss which can happen very early after having the crown put on the implant or it can happen many years down the road. Dental implants are fantastic, but nothing is without risks. If your dentist tells you they are 100% successful and have no problems ever, I would suggest seeking another opinion.
This condition is difficult to treat. Fortunately, most patients never develop this.
Most patients are unaware that they have bone loss around the dental implant. Peri-implantitis generally progresses in a painless fashion. Once it is established, you may begin to develop symptoms.
There are several risk factors. Smoking definitely causes constriction of blood vessels which leads to bone loss. Medical issues such as diabetes, osteoporosis and poor immune systems are more at risk for developing bone loss around dental implants. If you have had gum disease in the past, you are more at risk. Your home care is critical… Brushing twice a day for 3 to 5 minutes with an electric toothbrush, flossing once a day and using adjuncts such as a rubber tip need to happen every single day… Forever!! Grinding your teeth is another risk factor for dental implant bone loss.
Of course there are surgical factors that cause peri-implantitis to happen:
Soft bone, lack of tightness when the dental implant is placed, bone that was grafted in a vertical fashion, implant size too big, overheated bone, and many others.
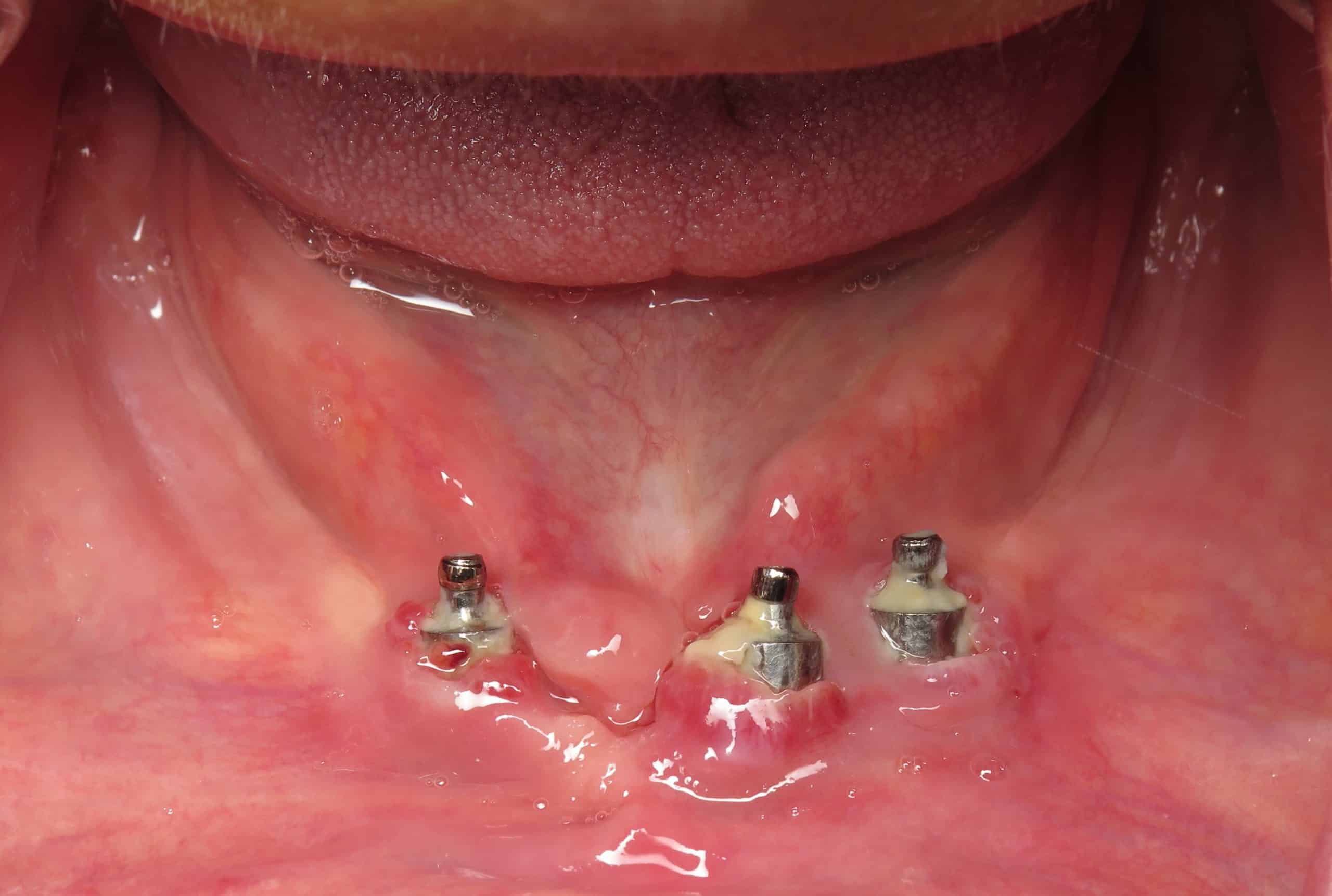
Signs of peri-implantitis
- gum pockets deepen
- pus comes out from the implants and gums
- bleeding at the gumline
- appearance – gum is red, or slightly purplish bluish, tartar/plaque build up
- progressive loss of supporting bone on x-rays
- metal thread exposure
- long tooth
It is not always symptomatic and typically there is no pain. Some of my patients have complained of dull aches or tenderness when they brush or touch the area. You can also develop a bad taste if pus has developed. If it is very severe, the glands in your neck may become swollen and you may even feel the dental implants being loose.
Who Should Correct Your Dental Implants?
I treat many patients with this problem. Unfortunately many of these patients had implants done with inexperienced dentists or large supercenter practices. Correction of dental implants with problems should be performed by a dentist who routinely performs this procedure.
The first thing I check for is to make sure the crown or bridge was made properly. The x-ray tells so much. Sometimes a 3-D scanning is necessary to see the inside surface. Extra cement is often the cause of peri-implantitis. The cement oozes beyond the abutment and gets down below the gum near the bone. The cement becomes an irritant. There is often good reason to make crowns held in by screws rather than cement in some cases. The technique of cementation and choice of cement used is a big factor on whether or not this will become an issue for you. You would be surprised to know that most novice dental implant dentists are not aware of proper cement choices although they have no ill intentions just lack experience and knowledge.
Occasionally I will find a loose abutment screw which may not have been torqued properly or it broke. That can be caused by someone with a really heavy bite. Patients with heavy bites need to have their crowns designed to protect the implants. How the crown is made is ultra critical for the longevity of the dental implant in the bone. So many patients view this step as minor, but it is major. Some low-budget implants have poorly designed screws or have micro motion when you chew.
Sometimes we find gum disease on other teeth just nearby which can stimulate peri-implantitis to start on the implant. Generally some type of exploratory surgery needs to be done to find out the cause and do a simultaneous bone graft in an attempt to save the implant. Not all implants that have peri-implantitis can be saved.
Normal Implant Bone x-ray (Implant by Dr. Ramsey Amin Burbank, California)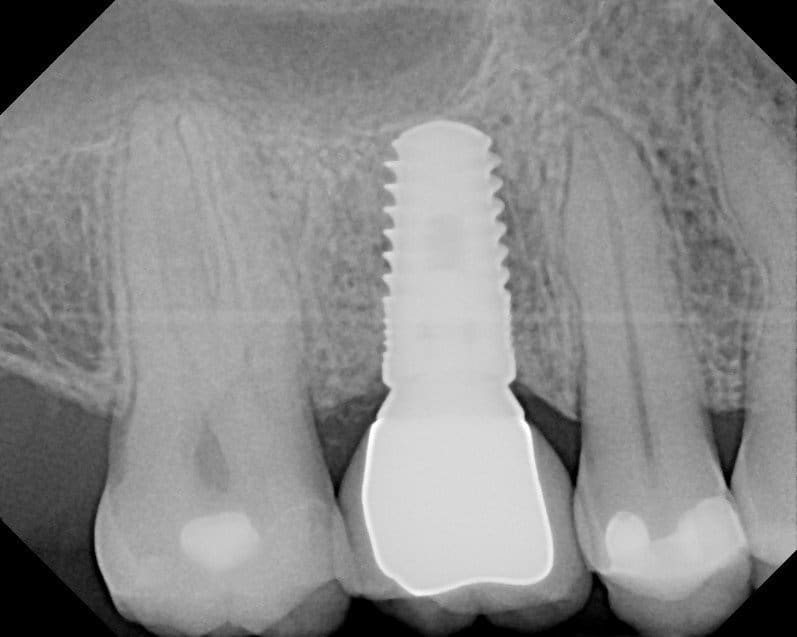
Treatment
The long-term goals are to stop the progression of bone loss and maintain your dental implants! Generally speaking the area will need to be cleaned thoroughly using dental instruments. Oftentimes antibiotics will be prescribed and special antibacterials will be applied to the implants itself such as iodine or tetracycline.
Most peri-implantitis dental implants require surgery and bone grafting. This means that your gums have to be opened and the area has to be detoxified. All of the bacteria must be killed in order to have bone regrafted onto the implants. I will definitely place you on antibiotic after this procedure.
The physiology and the type of bone that is used is critical. I would also suggest using your body’s own helpful blood products such as PRF/ PRP.
Time will tell if the procedure works. There are no guarantees on grafting around implants that have pre-existing bone loss. It is far more successful if the bone missing is in the shape of a moat rather than an entire wall missing.
Over the last 14 years of placing implants, I have developed many techniques to avoid this from occurring. When it does occur I have also developed techniques that seem to be more predictable. I have successfully regenerated bone around many implants over the last 14 years in practice. We have to be realistic when an implant has had too much bone loss though. The success rate can be as low as 35 to 50%. Some severe cases of peri-implantitis are better off removing the implant and placing a new one.
Just because one implant may have failed or develop bone loss, it doesn’t mean the second one will.
Please feel free to comment or ask questions below that are relevant to this post.
Floss!
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry

Thank you for this wonderful, enlightening article. My mother needs a front implant and is planning to go to her regular dentists for the procedure (Kansas). I was trying to convince her to seek out a periodontist. Is there any specific reason I can give her regarding why she would benefit to seek out an actual periodontist versus her dentist who says he’s “comfortable doing an implant”?😩
my favorite:
Full Mouth Dental Implants for Seniors: My Mom/Dad Needs Dental Implants
Hi Dr. Amin,
I’m wondering if you can help me. I had implants placed #7-10 in 1999 when I was 18 years old (I’m now 41) as the result of a car accident. The crowns are metal infused and are one piece. Over the years, there has been bone loss and tissue loss around the implants where you can see the exposed implants. I’ve always been self conscious of my smile worried someone will see the exposed metal. My dentist never had me get checked out. It was only after I started having discomfort with the crowns in the back (there is a large gap between the top of the crowns and my gums) that I said I wanted to get it checked out. He had NO referrals for me and I’ve been on my own trying to find a periodontist or oral surgeon to help me. Of the ones I’ve gone to, I’ve got mixed messages from doing nothing at all, taking everything out and restarting, adding tissue, adding tissue and bone, vestibulplasty, removing the sharp edges on the implants, just make larger crowns to cover…one said it could take 8 procedures…another one only 1 procedure… and most have said that they can’t get the implants entirely covered. To say I don’t trust anyone at this point is an understatement. What I really want is to get this corrected by getting the implants covered and then change out the crowns if needed so everything fits correctly when I’m finished. I want to do what it takes for that to happen. I’m still a young woman and I care about my oral health as well as the looks of my smile. The car accident was a traumatic experience, but this entire process of seeking restorative oral care shouldn’t be. Thank you in advance for any help or guidance you can provide. I’ve uploaded 3 x-rays that were taken recently to show you the condition.
https://drive.google.com/file/d/1BsBbl6n54h3jPhYrR7YhwqUY4jweIHWy/view?usp=share_link
https://drive.google.com/file/d/15t9Mx61B0QniK8GTqndk3JGDB4UhkWC6/view?usp=share_link
https://drive.google.com/file/d/1sASsEIkdNAFRRbg-fT6cvf4t8JMqO_7S/view?usp=share_link
Thank you for posting the images. There is no right answer or your case. Besides seeing your x-rays I would need to see you as well. Regardless you have a difficult situation. It looks like this was very well done at the time. So much has changed with implant technology to be more biocompatible with the gums. Less focus is on the bone and now the focus is on the gums.
Grafting bone back onto these particular implants is not going to be successful. This is a 360° defect. You are going to be best either adding gum to patch itor starting over. There are many cases I do just like this where I removed the old implants in place new ones right on the same day and make teeth on the same day as well. You are really going to need to see somebody who is a true expert in your area on this case.
Unfortunately dental implants are not permanent but they can last a very long time.
Hi Dr
I got a 4 implants bridge
Which all shows crestal bone loss and papila loss
It’s very uncomfortable especially when brushing there is pain
Per x-rays and cbct all says implant are still good and just do maintence
I am really uncomfortable
What can be dkne
I would need more info to really help here. Are you using a waterpick? Will a gum graft help?
Dear Dr. Amin,
Information you have given us has been very helpful. Having a whole host of issues,i.e. JRA, Osteoporosis, night grinding, and poor hygiene ( which happens when you’ve got so many other health issues). My new dentist has shown me that my bone around my multiple implants has deteriorated a great deal. Are dentures today look pretty at all? I am only 56 and really stunned about this news. What are the options if all else fails?
Hi Mary – Sadly, I deal with these types of cases on a daily basis. In short, the remaining teeth and implants can be removed and new same day implants or dentures can be placed. You need to see someone who is really good for revision. Things can be successful if done differently. There are many solutions that will last without going to dentures 😉
Dr. Amin,
Can type 2 diabeties be the cause of implant failure? I have had one sucessful implant and two that were done with a different doctor at the same time that failed. I am concered about where to go from here?
Yes it is possible if your type 2 diabetes is poorly controlled. Implant failure is more common in somebody that has an elevated A1c especially over 8.0. Other comorbidities such as smoking, steroid use, use of antidepressants/SSRIs can also increase risk of implant failure. Also implants feel more commonly in the upper jaw than they do in the lower jaw. There are many many reasons. I would suggest you see somebody who is very skilled and can manage her risk factors.
And each implant site is not created equal. Even in the same person one area to another can be vastly different. I hope this helps. Please reply that you received this
Hi Dr.
Thank you for this informative article. I am nearing the end of a two year full mouth reconstruction…..my second in 8 years. The first was done wrong, all 28 crowns were ill fitting and left wide open margins leading to severe tooth and eventually bone infections. The VA tried to save my teeth, but only 10 on the bottom were salvageable. I have had every other tooth surgically extracted, multiple(so many) bone grafts and I’m 13 days out from the worst surgery(for my mouth) I’ve ever had, and it was #16. 11 teeth, all that were left on my top arch were removed, 6 implant bases and much grafting we’re placed and I’m without teeth for 3-4 months while it heals.
My question, if you have a chance to respond, is this: my god, how long will this throbbing aching pain last? I have cried every single day since the surgery, 7 hours under general anesthesia in the OR. Swelling is mostly gone, stitches just fell out yesterday, but I swear they lifted my nose up and stitched it back down during this surgery. My sinus was punctured and my nose bleeds every time I sneeze.
I also posted this here so people will know that this is not a quick, easy surgery. It is painful and exhausting.
Thank you.
Without teeth for 3-4 months while it heals!!! Yikes! Even in the most EXTREME situations such as quad zygoma implants I still provide teeth in 24 hours! And very little pain.
So sorry. I hope your pain goes away quickly. Steroids, Arnica, ICE, PRF and antibiotics are always a help.
I would suggest MOBIC (NSAID) plus tylenol for pain at the same time.
hello Doctor
I recently had a failed case, the implant was placed two months ago but was taken out eventually.
What happened was that I had infection. My dentist cut my gum open and checked but he said that the infection did not happen on the implant body, it’s in the side area, so he cleaned the area and left the implant inside. He also performed bone graft at the same time.
Unfortunately, after two weeks, my dentist had to take the implant out. He said it failed but it was not because of the infection. (I started taking antibiotics after the infection.) It failed because the surrounding bones were dissolved or disappeared. It caused the entire wall of bone disappear for one of my neighboring, healthy tooth, and I think it is extremely unlikely to have bone grow back, so this healthy tooth will end up dropping very soon.
My question is, aren’t bone graft supposed to generate bones? How can the bone graft surgery make my bone disappear in just two weeks? (bone entirely gone). Is this normal to happen? Is there a way to save my healthy tooth that loses one side of bone?
Yikes. This is a really bad scenario. My guess is that you probably already originally had some sort of periodontal disease or bone problems on the adjacent teeth but that should speculation. Bone dissolving away is evidence of infection typically or something else we call necrosis. Regardless this is going to be very challenging to reconstruct. Bone grafts are supposed to generate bone but do not always. I also suspect that perhaps your case was more advanced and than this particular dental office has experienced in. I would suggest he see somebody whose an expert in this arena to help correct all of this. It will probably be a bit slow going to get it all repaired. It is possible you may lose adjacent teeth. I am hoping that you do not smoke?
hello Doctor
I don’t smoke. I visited two periodontists this week. One of them said that she will try her best to perform bone graft & gum graft for the missing tooth (#19), and it may also help support the adjacent tooth (#20). As she is one of the best in Austin TX and my 2nd opinion dentist recommended, I’d go with the treatment plan.
But she also warned me that, even if the bone graft achieves the best outcome, I may still lose the adjacent tooth in a few years or even less (originally keeping 10 years should be fine), as the bone cannot grow vertically.
I talked to them about taking part of the bone from my body and attach to the adjacent tooth, but they said that they did not see many practices doing it in recent years. They’d suggest me to talk to an oral surgeon.
What I am thinking is that, after the periodontist helps grow my bone to certain level, is it possible for an oral surgeon to take part of bone from my body to support/attach to the #20? I have the X-Ray of the tooth (#19 & #20): https://docs.google.com/document/d/1pUwniVQfE0F_NXPWkr11OVEfMJE4DtC4lAq-ULaeMDQ/edit?usp=sharing
Thank you
I was able to look at the x-rays. I think the software position the second x-ray is not correct making the bone loss look worse than it really is. How we position the X and Y axis In the software can make the bone loss look worse or better. With a single image I don’t think it’s correct because it does not really match the regular x-ray above
I think you should have your white checked carefully for fremitus. My guess is the bike is too heavy and if it is reduced or eliminated you should be able to keep that tooth for a long time
Often the bite might get too heavy when the molar behind it has been taken out.
I had to have #13 and 14 pulled. Later a sinus graft and a Bicon implant placed. My dentist placed the implant where #14 had been and is going to make a double “bridge”, that is 2 crowns joined together, attached to that one implant. We talked about it beforehand, but my understanding was that he would center the implant to more evenly support both crowns in the bridge. Is it ok to put the implant just over one tooth and expect that to support both crowns evenly? I’m afraid a short Bicon will break as there could be more micro-movement from #13 which isn’t anchored (except by the implant at #14). I go for impressions in 3 weeks so really appreciate your insights!
One implant for 2 teeth is fine in some situations on the FRONT of the mouth.
But for back teeth, this is too much force Laurie.
Are your sure this is the plan?
Sorry for the delayed reply. Busy month! 😀
Thank you for taking time to reply; no problem about any delay! I really appreciate your opinion! We had moved a few years ago but I am going to go back to the periodontist who did 2 lower implants 8 years ago. He is farther away but said he would do 2 implants to replace those two back teeth (not just one as the other dentist wanted to do) Yes, I know the first dentist planned only one implant for a 2 crown restoration. It was also in my written treatment plan. But I did not feel it was right and I really appreciate your opinion!
🙏😊
How can I find the right dentist. I have had an implant 7 years on #30,
now I have extensive bone loss, No pain, gum recession on the cheek side has always been there. I am a healthy person.
The tooth 40 years ago had a root canal. 20 years ago it broke and I had a crown lenthening.
Before retirement I was willing to replace it with a dental implant.
I changed to Comfort Dental. Once he had me take an xray to the dental implant dr. , no appt. was made but he looked at it and commented. A little bone loss at the time to be expected. Keep up with cleanings and examinations.
I continued with cleaning at Comfort Dental, but the Dr. there would never look at my teeth cleaning and xray. He wasnt available. I decided to not go anymore. I am back after two years. Now he sends me to periodontist. They just want to take it out. He said nothing to graft bone to. My tooth feels ok and I am now using coconut oil on the side to help the receding gum. I feel ok. Can I just do nothing? I mostly want to stop the bone loss.
Unfortunately once a dental implant has substantial bone loss it is likely to be progressive. 🥲
If it has more than 30 to 50% bone loss you should remove it sooner than later. The sooner you take it out the easier it will be to replace and destroy less bone in the process.
About 30% of what I are revision dental implant procedures.
Dental implants are still the best way to replace teeth. If you’re considering having it done again I would be sure to see somebody with a lot of experience to help avoid this
Having healthy gums and plenty of gum tissue around the implant will help long-term stability and keep the implant for 20 to 30 years
https://burbankdentalimplants.com/service/failed-dental-implants/
https://burbankdentalimplants.com/gum-graft-transplant-for-dental-implants-is-it-necessary/
I have a question dr I did an implant surgery back in November 2019 and all the 3 are ok except one it keep getting infected did bone grafting 2 time and I’m going to the 3 surgery soon not sure what’s the problem please if I can get any advice please .
Can you share an X-ray and photos publicly on google drive?
Hi Dr. Amin, I had the bottom left two implanted teeth (two years ago) that showed some bone loss. The dentist suggested a soft tissue surgery with bone graft. Do you think this is the right way to go? Do you think there is a better alternative? Here is the picture: https://drive.google.com/drive/u/0/my-drive
Thanks and I would really appreciate your opinion!
dead link
;-(
Sorry Dr. Amin, I am not very good with the file sharing. Here is the copied link again and hope it works this time. Thanks a lot!
https://docs.google.com/document/d/1CaGXHDbqYPyxWcVme1UQuXVT6gF_GoiTs2a9TWmThMk/edit?usp=sharing
I saw the images!!! 😉 The gum graft is likely more beneficial than the bone graft. But it is worth doing both in your scenario. Even if the bone does not take, the gum should stabilize it from further loss!
Hi Dr Amin,
Thanks for this very helpful article! I was recently diagnosed with bone loss around my left lateral incisor implant (placed in 2013 after an accident where I lost the original tooth). I had it placed in Australia where I am from, and am now seeing a periodontist in the US. I first noticed slight gum recession and a purple-ish gum color, but no other symptoms. The doctor I saw noticed I have excellent oral hygiene (twice daily brushings, flossing, regular cleanings), so I am concerned that this happened in the first place. I do have a night guard to protect the implant from teeth grinding. I do not smoke or have any other real risk factors that I am aware of.
He is recommending a bone (cow bone) and gum graft to restore the bone loss and improve the slight gum recession. What is your opinion on this?
I am also concerned about getting an aesthetically pleasing result given that it is in the smile line.
PS- I would love to come and see you but I am based in NY at the moment!
Thank you for your very kind words. Often times a revision bone graft and gum graft can help improve things. The most critical area is the triangle of gums. In some situations the surgeries can make it worse than better. Obviously do your due diligence but it is a common procedure to try to correct your issue.
Thank you Dr Amin! If there is already some bone loss occurring, is it better to re-do the implant altogether rather than trying to correct it through what is a complex/unpredictable procedure?
Hard to say without seeing you. 🙁. Sorry
Thanks, Dr Amin! I would love to try and see you when COVID is over- hard to travel from NY right now… thanks again for your help.
Hello Dr. Amin, I have some bone loss around my two 8-year old implants. The oral surgeon that I saw recommended implant removal, bone grafting, and new implants. I guess I have too much bone loss such that it’s not possible to do bone grafting without removing the implants. I did some research about this oral surgeon and the reviews are not that great. I’d love to see you but I’m in Virginia. Could you please recommend a great implant dentist who is experienced with this problem in Virginia or Greater Washington DC area? Thank you so much.
How to find a great implant dentist.
~stay safe during COVID 19
Thank you Dr. Amin. I really would like to have your advice and if you think the removal is the only way, I want to have it done by you. Would you provide online consultation where I send my X-ray and other required information?
Please contact the office to set this up.
I had a similar problem to you. I removed my implant and did bone grafting then a new implant.
Thank you for the very insightful article! I hope you are still answering questions at this point.
I had implants done in tooth #13 and #14 in 2014 and 2015. I relocated, and during a routine exam with a new dentist, x-rays showed bone loss around both implants. My dentist referred me to an endodontist who performed laser surgery to clean out bacteria and strengthen the bone. He’s been very pleased with my recovery, and now at the 6 month point, he sees some regeneration in the bone.
My issue is that I now have some gum recession and a larger gap between the two teeth that is very bothersome. My tongue seems to land in that area so much so that I’m conscious of the gap. I also worry that I might crack one of the crowns with food getting in there when I chew, even though I’m extremely careful and the endodontist said I’m doing very well with hygiene and keeping the area clean.
Is this recession a common occurrence with laser surgery? I thought laser surgery was supposed to minimize gum recession. Could something have been done wrong with the procedure? Or could this have happened due to the complex situation of having bone loss in two adjacent teeth?
I had another surgery for root canal that was done traditionally, where I had 8 stitches, and I had no gum recession there at all. I would love to hear your opinion.
This is really an excellent question. Any type of surgery meant to correct a dental implant losing bone is likely to result in some gum tissue loss. As the area becomes healthier, the swollen unhealthy gum shrinks leading to some recession and oftentimes opening on adjacent teeth. Is not likely anything was done wrong it is just that the implant may need to just come out and be replaced. Often is not worth keeping a failing implant if it has begun to affect the adjacent teeth.
Thank you for your quick response, I really appreciate it!
The 2 implants are adjacent to each other and it’s the gap between them that has grown. None of the two adjacent healthy teeth on the other sides of the implants have been affected.
Hi,
First of all, thanks for this article! I have found it difficult to find information on how to fight peri-implantis.
I have recently had 7 implants placed due to genetic hypodontia. I was missing the 4 bottom adult front teeth and had 3 baby teeth there originally. I finally decided to go under the knife before I lost the baby teeth as I’m now 24.
I have now had 4 implants on the upper jaw with one bone graft, these are all healing well and will be having permanents placed in a couple of weeks.
I had 3 implants put in to replace the 4 missing bottom front adult teeth, I had an artificial bone graft to build up the jawbone as it hadn’t developed fully. I am now about 4 months post surgery and I have been told I have bone loss around the bottom 3 implants that mean i need to keep my temporaries in for now as it isn’t strong enough for my permanents yet. My dentist hasn’t said/prescribed anything and has just said we will assess at a later date. I’ve not found anything about loss of bone after a bone graft and implants, is this something I should be concerned over and seek another opinion? Is there anything I can do such as calcium pills to try and nip it in the bud so the bottoms will heal quicker?
Thankyou!
Rebecca
I am sorry I missed this old question! How did it all work out? Dr. Amin
Hi there,
I have had my implant for over 10 years and almost always had a fistula by the area. I had it checked out and they said to continue to monitor it. My last check up, it was noticed that I have a 7 pocket around the implant and that there was bone loss such that the gums are below a couple of the implant threads.
In my discussion with my periodontist, she said that she could do flap curettage, but depending on how it heals, some of the implant may be visible. Since this tooth is next to one of my front tooth…I’m a bit concerned. I’m not that interested to have a mouth of white teeth…and a little piece of metal showing.
I asked about the bone graft, but she said bone grafts were a waste of money and that my best options were LANAP or flap curettage. For the cosmetic remedy, I could have the cap removed and replaced closer to the gum line; but that would mean replacing the crown and attachments to the implant (currently held in by glue). I’m going to get a second opinion from the periodontist that put in the implant…but I thought I’d ask you.
Are bone grafts to build up loss bone around an implant a good idea? Does it work?
Thanks,
Mike
it works….sometimes….the conditions and treatment have to be ideal. Because the dental implant does not have any live blood supply sticking gum or bone onto it is more difficult because it is not alive. Oftentimes I take my carbon dioxide laser to treat these areas.
if the defect is not a 360° moat…. Then it just may work. Salvaging/rescue work is more challenging than complete replacement.
To cut a long & painful experience short, thanks to a very swanky and expensive dental practice who did inadequate check ups on me for years, (I only know this with hindsight now), I had serious issues and needed extraction and 2 implants. I always cleaned and flossed well. I had good oral hygene. It was their poorly fitted crown and decay behind another back crowned and root canalled tooth that did the damage.
I went to a specialist practice to have the work done. No way would I let the previous imo negligent surgery do it, eventhough they had so called “advanced techniques” & all the equipment you could think of. Not after what they had done to me.
My new chosen implant clinic has been fantastic. They had a lot to do on my mouth for the abcess & upper bone decay above the 2 teeth they extracted.
Here’s the weird bit. The back upper implant despite all concerns took after a sinus lift and plasma insertion. I know I have to take care with it but the new bone growth seems to be going great. It feels secure.
Unfortunately the canine front implant, the one that had a sudden, whopping access directly above it before the original tooth was removed, rejected. This wasn’t expected as the bone left seemed to provide a tight fit when the implant was inserted. Not only that but the x ray was horrifying to see. The bone had significantly diminished around the implant. After the tooth extractions the implants weren’t put in for months so it’s not as if anything was rushed or compromised. I also had anti biotics after the extractions.
I was told I could have a bridge as I have cosmetic crowns either side, or I could wait 4 months, just to see if by some miracle, my own bone would grow back. It wasn’t expected to at all but at least I could take some time to see if I wanted to try a graft.
I have a healthy diet anyway and include fish oil, an array of green vegetable powders and home blended fruit & veg drinks. I continued with these but also added things like powdered organic kale, broccoli, vitamin K2 & a higher daily dose of vitamin D3.
To everyone’s amazement, my bone was growing back. Not only that, it’s strong, but flexible, not brittle. It’s continued to grow around the new implant at a rate no one can fathom. It’s been like winning the lottery for me.
So for me, keeping up the fruit & veg blends, green powders, chelated calcium, wet fish & shellfish derived collagen, vitamin k2 capsules derived from tofu, hyaluronic acid tabs seems to have worked. Wild krill oil capsules were added to my regime too.
In my view, diet absolutely has been a game changer in my personal experience. From little hope for 2 implants to hopefully, after nearly 2 years since the nightmare started getting 2, God willing, strong, successful implants.
There’s some good advice on the web about How To recover from bone injuries. I took that advice. To me it’s obvious, your body can only heal as much as it can given what you eat & drink.
my DDS wants to do flap entry/CL and look at my implant, #10 upper left front. X rays showed slight bone loss 1 thread exposed.he said he leans for cleaning and smooth out thread instead of bone graft depending on what he sees . the implant next to it is great, no bone loss ? should I get this procedure done. 9 years since the implant was put in.
hmm…front tooth…may look worse after procedure…that is the issue. Discuss this with the DDS
my smile does not expose my gums so much, he said doing a bone graft the gums would shrink more then doing a cleaning, acid wash. he leans more for deep cleaning.this will also be exploratory and he and I can make the call.can deep cleaning stop the loss of any more bone.
hmm…front tooth…may look worse after procedure…that is the issue. Discuss this with the DDS.
Hi Dr. Amin,
2 years ago, my then 17 year old daughter had a mini-implant on #6. She was born without her primary tooth thanks to genetics. Within a few months after the mini-implant, the tooth became purple and dark and at the gum line and loose. We went back to the dentist that performed the procedure and was told it is part of the healing process. A second opinion showed bone loss in the ex-ray at the site of the implant.
I took her to a specialist for evaluation and the bone loss diagnosis was confirmed and was told her mini-implant was failing. She has since undergone a bone graft and we are waiting for that to heal before a long term solution is done. Probably another implant (not mini).
Can you give me your expert opinion on:
1. what might have caused bone loss in a otherwise healthy 17 year old girl, after having received a mini-implant?
2. Mini-implants in general.
Thank you so much.
Michael
Miniature dental implants unless placed in a super narrow space would be considered temporary. They can be used for lower incisor teeth or some very skinny lateral incisors but typically placing implant in the #6 position should have a larger implant. Bone loss around implant in her situation is difficult for me to answer without seeing her. In general I try to delay dental implants on young patients until they are in their early 20s at the minimum
Thank you for your response. I made a mistake on the tooth, it’s #10 and not #6. Please comment if it makes a difference in your original reply.
Thank you again for your time.
Hi Dr. Amin,
Thank you for this helpful post, and for your blog in general. Had a question for you, as I am considering a few options.
i had an implant placed a year ago (December 2017) on #30. The site originally had a root canal that became badly infected. They extracted the tooth, cleaned it, did a bone graft plus implant the same day. I don’t live close to the dental office, so they gave me the option of extracting the tooth and coming back later for the implant, or doing it all that day. I chose doing it all that day.
Fast forward 3-4 months, in March this year I felt some sort of bulge on top of the gums that continued on and off throughout this year. No pain. Sometimes puss would come out.
I just got it checked again yesterday at a periodontist here in San Francisco, They measured the bone level after anesthesia and the periodontist noted that the facial aspect of the implant was missing about 8mm of bone starting from the top of the implant, about 2/3 of the front of the implant didn’t have bone.
His prognosis was that the implant was failing with peri-implantitis and the recommendation was to take the implant out, put new bone graft in and let the site heal for at least 3-4 months before putting a new implant in again. He had a strong opinion that it wasn’t the best move to put an implant in the area immediately when there was originally an infected root canal.
I’m going to be speaking to the original surgeon in the next few days – as of now based on the x-ray he saw, he thinks that we can save it by doing another bone graft, but he wants to come back and do a 3d x-ray to assess if it’s possible to do. Here’s a picture of the x-ray I just got yesterday:
https://drive.google.com/file/d/17rNvCvSeiS30D8aD62I2wpypACIAierx/view?usp=sharing
I am currently taking amoxycillin for 7 days and deciding what my next step should be. The periodontist I saw yesterday was quite opinionated that I should have my original surgeon remove it and start over, but reading your post here has me thinking whether I should try saving it. It would not cost me anything to try and save, and it wouldn’t cost anything extra to have it removed and re-done either. It is covered by warranty for 2 years.
The issue is more time driving back and forth (it is 10 hours from my home), the hassle, but also trying to balance what is the best long-term move.
Your thoughts would be appreciated. Thank you!
thank you for your kind words. I hope I can help. The best option would be to remove and replace it rather than try to rescue the implant. very nice that you uploaded a Google drive. I wish everyone else would do this!! It does not look that bad on the x-ray but the clinical examination is most important. The fact that you’ve had symptoms with an infection is obviously not a good thing. Replacing molars with dental implants on the same day of extraction is very routine for me. They can be placed in areas of chronic infection but generally not acute infection. I don’t think you had any poor treatment just an unfortunate outcome. This should be very simple to replace. Good luck. I think you also contacted our office as well 😉
That’s helpful! To follow up on that…
1) Based on what I said, would you say I had an acute infection then? I had an infection in the area at the time of procedure. But it had been going on for months.
2) If I were to replace it, is it possible to pull out the implant and put a new implant in with a bone graft on the same day? Or do I need to pull it and put bone graft, and then wait 3-5 months for it to heal before putting a new one?
3) If my original surgeon is persistent about doing a bone graft to save it and I end up doing that, is the implant’s long-term lifespan declined because of the peri-implantitis, or is it possible for it to be good for a long time if the bone graft is successful?
Thanks again for all your help. I will be getting a second opinion most likely up here in San Francisco before going to the original surgeon again. Maybe I will come down to Burbank as well since I have to go to So-cal in January!
1. Can’t answer without having seen before the tooth was removed
2. Sometimes it is possible for same-day replacement often it is best to just wait especially if it is towards the front
3. Am going based off of memory but a new implant always performs better than one that is rescued in most situations
4. Oftentimes a tissue gum graft is really needed to thicken the area and prevent future loss of bone
I had my implants started in 2017 and finished around feb or march 2018. I had to have bone grafting done due to bone loss. About 4 weeks ago, I started to feel throbbing and pain in my one implant area. I had implants placed for both of my front teeth. The tooth bothering me is my left front tooth. After about 2 weeks of progressing pain, I saw my dentist. This was about 2 weeks ago. They did xrays and said everything looked good. Said my gum in that area was puffy and bleeding. Told me it’s possible something got caught causing inflammation. My crown was slightly loose then. I was given antibacterial mouthwash and told to use it daily and I have. The pain started to subside but my crown became loose. I meant to call today to get in but work kept me busy. Tonight as I was brushing my teeth, what appears to be my crown, abutment and implant all in tact came out.
I am a bit worried as I cannot afford to pay for this to be redone. Also, because I felt the reason I was given at my dental appointment didn’t seem right. I, unfortunately, have had multiple dental procedures from a young age. This particular tooth I had a root canal in high school and 2 or 3 crowns that failed and multiple recementings before implant. What do you think maybe the best course of action.
yikes!!!!!!!!!!! a dental implant placed in 2017!!! are you saying that the screw part in the bone fill out as well? It seems impossible that you can have an x-ray two weeks ago showing the bone is good and then for it to fall out. I’m guessing maybe it is just the crown and abutment that can be replaced just by tightening the screw or replacing the cement. Hopefully all is good and implant dentistry has not let you down. Keep in mind that dental implants have a very high rate of success both short and long-term. Problems that you are all reading here are the exception rather than the norm. See the best implant dentist that you can that has the most experience
I had an implant places 5 years ago and have recently developed bone loss around the implant. A pocket developed and has filled. I went to my general dentist and he proscribed antibiotics and contacted the provider that placed the implant. I have an appointment in a few days with the provider that put the implant in. My concern is the cost associated with treatment. Typically do dental providers correct the issue on their work at no cost, similar to a lifetime insurance on parts and labor?!
This is a great question. It is impossible to truly predict this will occur on. In my office if it occurs to a patient that has had an implant less than 1-2 years I often take care of it at no cost if they do not have a medical or lifestyle issues that has caused this such as heavy smoking. 5 years out is not likely to be a covered benefit. I wish my own body had lifetime insurance!!! 😉
I may have implants soon.
Please tell me how you have regenerated bone around implants.
LIPUS i understand may do it. Please comment on this.
Thank you
I don’t understand your question. In some cases it is very possible!
Doc. I was just treated for peri impantitis. I am 5 post op and still in a significant amount of pain (5 out of 10 while on ibuprofen and 8 without). Taking 600 mgs ibuprofen and erythromycin as prescribed. My bone loss was “moat” like and my specialist was confident he could get the mass back with the bone graft.
1). How long does the pain generally persist with this treatment?
2) What is the usual healing time and
3) what are the odds that this treatment will need to be repeated.
Thanks so much!
3-21 days ———1). How long does the pain generally persist with this treatment?
6-12 months to see if it worked………..2) What is the usual healing time and
Difficult to answer…widely varied…………3) what are the odds that this treatment will need to be repeated.
My wife has a few implants done about 16 years ago , she has never had any problems but on the last visit to her new dentist just for a check up he recommended a clean etc, during this my wife complained that her implant was knocked and felt pain the operator told her it would subside in a few days, if fact the pain got worse and returned to the dentist he recommended drug treatment , but it has not cured the problem, can you sujust something please
hmmm…perhaps seek out a specialist in implants.
I had zygoma implants (two on the left and two on the right) done on June 18, 2018. Everything appears to be going well. On my right side under my eye I notice a tingling and some numbness just below the corner of my eye. There is no movement with the prosthesis. Is it normal to have this feeling and do you think it will eventually subside?
Thank you for your time
Since it wasn’t done that long ago, it will likely resolve with time. Zygomatic implant placement can result in this.
Hello Dr. Amin,
I am 53 years old and had dentures since my mid twenties. I also have osteoarthritis. I had two dental implants done today without major problems. But then they started to work on my bottom right side. There the problems began. Bone was extremely weak. Dentist tried implants and put them out to get another size and screwed them in. They had to be taken out as well. Next she did bone grafting and put a lot of bone in. It was getting late and I drove home, and oh my god I was in so much pain. I literally cried, and I am not a crybaby lol. Tylonol 3 did not do a great job. Stayed up for hours and prayed the pain would go away. Now I took my second Tylonol 3 after 6 hours. Thank god it seemed to take effect. Will I feel terrible in a few hours again?
Thank you for considering my question
Susan
There are ways to do this with little to no pain…even with large bone grafts. Ibuprofen is much better than tylenol for dental pain if you can take it! Sorry!!!!!!!
Hello, I am a 70-year-old woman. I have had dentures since I was 18 years old when a dentist pulled my teeth telling me it was so best thing Do at the time. I have a full upper denture. By the time I was able to afford implants a dentist put a 10 or 11 mini implants in my mouth to hold my upper denture and then he glued it. I didn’t know that this was not a procedure that was done often. He retired and I started going to another dentist. Now I am told that I have a bone loss at 50% and I have one implant starting to go through The naval cavity. I was told That I had to have all of the mini implants removed and both grafting immediately. After the bone grafting I could have regular implants placed and I could have teeth that would be fixed. I just read Your article saying that you can go in and clean out the entire implants and possibly save the implants. I am not a rich woman, and no matter what procedure I do this will be an expensive thing.I would like to know is there a better way? Thank you
There are times where placing implants are intentionally into the base of the nose is extremely helpful. I do this sometimes of course with the patient knowing this in advance. Bone loss around miniature dental implants are not worth recovering. Replacement would be a better option. Rather than doing bone grafting I would suggest bone leveling and perhaps consider zygomatic implants over a sinus lift for a more streamlined procedure. This can provide you with immediate teeth on the same day of the procedure bypassing all bone grafting and going back to a denture.
Dr Amin,
I had an implant placed about three years ago at #19 with a bone graft. All went well until this week. I now have significant swelling at the outside gum at the base of the implant. I don’t notice any gum irritation or bleeding, My Dr immediately prescribed an antibiotic to treat the infection and scheduled an appointment within the next week. I am sure I will need very aggressive treatment and face a high probability of losing the implant. He is a periodontist as well as placing implants for quite a few years and I feel satisfied with the work he’s done so far (four implants). What should I reasonably expect as viable treatment or should I just have him remove the implant. Of course I am very disappointed, but I take the blame for the failure.
Sometimes this happens for no good reason at all. Just ask your dentist what the prognosis is long-term for a rescue/repair procedure. Depending on the pattern of the bone loss this can be very successful. It is only unsuccessful when there is 360° horizontal
Bone loss rather than just certain area of the implant
I had an implant placed at #26. It failed and was removed. The implant was literally swimming in infected bone and easily removed. The bone level dipped very low at that site after the implant removal. I had a bone graft done there, waited 6 months, and then another bone graft done before placing another, narrower implant. Unfortunately there wasn’t enough bone for the second implant to take either (it ended up with micromobility and the threads were being exposed with bacteria forming on the threads). Now I have had the second implant removed and a third bone graft (the bone grafts don’t achieve height at the #26 site and there i is a narrow but deep drop at #26 where the bone is missing.It appears that #25 and #27 aren’t compromised as they’re solid, but the gumline dips sharply down on the #26 side of those two teeth. #25 became slightly rotated from the initial implant bone loss). I was told they have to wait to see a cat scan had to be done to determine if if there is enough bone to do a THIRD very skinny implant but after the last implant removal/bone graft was done ten days ago, and it looks like much of the bone that was placed there is resorbed and doesn’t accomplish height; the dip in the gumline at #26 appears to be even a bit lower.
Sounds like a complicated lower front tooth. Sorry for all your problems. Grafting that narrow space in a vertical fashion is intended for an expert. Another option may be not to do an implant.
A Maryland bridge an option sometimes. If those adjacent teeth aren’t PERFECT, then the bone growth will not be either.
I hope this makes sense. See link.
https://www.burbankdentalimplants.com/sometimes-dental-implants-are-not-the-best-option/
it is lower left side next to last tooth. implant has been removed and bone grafting was done at the time of removal.
I had peri-implantitis and ended up having surgery. 13 months after surgery I now have a pocket at the implant site. Periodontist wants me to decide between having the implant removed and having indefinate treatment. He hasn’t given me enough information. If I am going to continue to have problems then I say remove the implant otherwise I need more info. I’ve tried to get more info from the peridontist but without success. I clean my teeth 4 times or more per day and floss. I also use the interdental brushes the peridontist insisted on. What do I get for this? another problem. it is so frustrating.
Super frustrating. So sorry you have to go through this. There is a small percentage of patients that requires retreatment. Sometimes the rescue/ salvage procedures are not worth it making removal and replacement becomes the best option.
is there a chance that another implant could be put in the same place sometime in the future? Now I’m being told that the implant might not be removed. Oral surgeon’s office says maybe the crown is to blame? Any info on the crown causing pockets and/or peri-implantitis?
Yes it is possible that the crown causes this. It would have to be a really bad crown with a poorly designed abutment or even mismatched and or loose parts.
having the implant post removed on 5/24/2018. I am angry, frustrated and scared. I had so much pain after the surgery for the peri-implantitis. I image this will be painful too
I had the implant removed and had a bone graft on 5/24/2018 by an oral surgeon. She said that she does not do the flap surgery that the periodontist did last year because it doesn’t work. I can attest that it did not work for me. There was very little pain with the removal. Happy about that. September the oral surgeon plans to put in another implant. then approx. 1 1/2 months later, she is going to remove tissue from the roof of my mouth and put it inside the gums to reinforce the area around the implant. Never heard of this and am nervous.
My daughter is going through a terrible time with an upper front tooth implant, to the point of becoming depressed. She just got her permanent crown on about three weeks ago and was complaining about some continuing pulse sensation and wanted her oral surgeon to do x rays but they said it all looked good and they didn’t want to subject her to needless radiation. She was pretty upset as she has talked about something not feeling right since they placed the crown. Well last weekend the puss began again around the gum line while she was visiting. I had her see my dentist on a saturday and they took x rays and said they were seeing some bone loss. She was devastated! She knew something was not right. The oral surgeon seems to be good but now she is nervous and doesn’t know if she should trust him. She has an app this thursday to have it cleaned out with a bone graph. She literally was able to bite into soft things for the first time in 9 months a couple weeks ago and now is going to have to go back to not being able to bite into anything. Will this take as long to heal as the original implant? and how successful are the clean outs and bone graphs?
Ugh…so so sorry for your daughters trouble. It is very hard to know what went wrong or if she is just a poor candidate for dental implant. Rescue clean out procedures with bone grafts have a variable success rate and there is no general consensus on how it should be done. Each of us has a different technique, different skill set and equipment for these cases. Hopefully everything works out well. Please keep us posted. Antibiotics are must for these procedures!
I have had an odyssey with my implants. I have never had a cavity but have experienced fractures in 18,19,30 and 31 due to grinding. I had an implant on 30 several years ago that integrated successfully and has been rock solid. On 19, I had the first implant that failed. We did a replacement implant and it integrated well but the cap screw could not be removed. The oral surgeon and my dentist tried everything and eventually in the process of getting the screw off the implant came loose. So, we tried another implant on 19 and did 18 at the same time. They both seemed fine but when it came time to remove the cap screw and put in the healing screw, 19 had failed to integrate. So, we removed and went forward with 18. We had no more problems with 18 and placed the crown last week. Almost immediately, I noticed a little pain when chewing on 18. It is only when chewing and only when it isn’t soft food. I spoke to both the oral surgeon’s office and my dentist. The x-rays show that there is bone all the way up and past the threads so it doesn’t look like bone loss. I am to see my dentist on Wednesday. My oral surgeon’s office said to just eat on the other side and see if the pain subsides. I know probably none of this is ‘normal’ but is there a possibility the my pain on 18 is just my jaw getting used to me chewing there again?
Wow… What a saga. I’m so sorry you have to go through this. It is critical that whoever is making the restorative crowns on the implant is designing them in such a way that when you’re jaw joint is fully seated in what we call centric relation that it does not interfere with your bite. This tiny detail can cause implants to fail routinely in this area on the lower molars. I am hoping that when you bite down you clear the healing abutments when there was no teeth on the implants. This all sounds very strange. I am assuming you are a healthy individual, no medications, no bone problems and a nonsmoker.
Hi Dr. Armin, I am a 51 year old non smoker. I do have an elevated A1C. I take Omeprazole, Metformin and I am on Zedia. I have also been taking vitamin D for low levels of that as well. I have an appointment with my oral surgeon tomorrow. We’ll see what comes from that.
So what happened??
Do you have bone loss?
Omeprazole has been shown to impair dental implant healing. Vitamin D is correlated to bone metabolism and of course possibly being prediabetic with an elevated A1 C can be an issue as well.
The implant failed to integrate. The X-Rays looked good but there was no bone on the implant when it was removed. I guess failed as soon as there was load placed on it. I discussed with my oral surgeon and we came up with a new game plan. I am now off the omeprazole. I’m changing what I eat and when to deal with the acid reflux without the aid of proton pump inhibitors. I’m also working to get in better shape to improve my A1C. We are going to wait three months and try the implants again.
Thanks for the update. Good luck. 👍🏻
A new year’s update for 2021. I have continued to get and have implants fail. My implant on 30 has begun to fail. I have had that one for 8 years and it’s the only one that integrated successfully. I have implants on 18 and 19 that I had placed last March. They look good on X-Ray but I had pain on 19 that subsided after a week around Christmas, I have an appointment with my Dentist today and I am going to see about getting a crown on 18 even though I have little confidence that it has integrated. I’ve had 6 implants on 19 and 4 on 18, I believe. My oral surgeon has been extremely generous with his time and patience in replacing these implants but I wish I knew why they fail. I really don’t want to end up with a partial denture for these 4 molars but I don’t know what else to do.
hmmm…. My guess is that everyone is seen on the bone and not on the gum. You likely need a gum graft taken from your palate and transplanted to the area to have a gum tissue. The key to longevity. It increases the deepness of your cheek that all the vestibule and create a tighter seal around the implants. The other thing this could be is the bite design of your implants.
Hi Dr.,
I just had tooth #5 extracted, a bone graft done, and implant placement all in one day, by an experienced oral surgeon. This was 2 days ago. The area doesn’t have any pain, but my lymph nodes under my jaw on both sides are extremely painful and swollen. I’m in Augmentin, and started it 2 days prior to the procedure. The procedure went well, no complications, and I’m due for a check up in 3 weeks. My concern is why my lymph nodes are now so painful and swollen. This happened the day after the procedure. Any thoughts?
I think you should go in and have your dentist look at you sooner.
What was the outcome?
Dr. Amin: I recently had a 3rd implant…farthest back molar on right side of jaw. It ached continuously and the gum was red. I went back weekly to dentist complaining something was not right. He said it was healing slowly but seemed fine. Nothing changed. 4 weeks from initial implant procedure, I went in for typical cleaning and dentist checked implant. Said there was a swollen red spot on cheek side. It was tender to the touch. I had also complained of a general feeling of malaise during this. Went to medical doctor who could find nothing wrong with me. Day of the cleaning, blood and pus were weeping around the new implant. Back to dentist. Had to see his wife (dentist also) as my dentist sick. She said the implant had a gap between the implant and the tissue and bacteria had caused infection. I’ve had 2 laser treatments and antibiotic pack last week. No change. Tomorrow is 3rd treatment. Wife/dentist tells me if this doesn’t work, implant must be removed. My question…should I even bother trying another implant in that region? I believe the tissue is thin as I had bone graft. Don’t want to go through this pain again. I also cannot understand why my dentist didn’t see something going on from the beginning. I’m convinced there has been a low grade infection all along contributing to the malaise and general weakness. Nothing has been said yet about bone loss, but I am concerned about bone loss in jaw and disfigurement…perhaps foolishly. Tired and scared at this point. Any thoughts or advice? Female 65 yrs old.
Perhaps try just removing the crown alone and placing a healing abutments back on. Maybe the crown is not seated well at the abutment level. If the pain goes away without the crown on then the problem is not the implant.
Hello Doctor! I have a couple of questions. I had to get 3 titanium implants placed after reversing extraction orthodontics. I am doing more research now, and am finding a lot of info/data on titanium implants and links to cancer and compromising one’s health down the road. I know there are ceramic (non-radioactive) implants available. I know these are more compatible with our bodies and tend to be better when it comes to mainiting bacteria at bay, hence, avoiding all these pero-implantatis issue. What are your thoughts on ceramic/zirconium implants? Can ceramic/zirconium implants eradicate the issue of per-implantitis? Thank you!
Titanium dental implants do not cause cancer. We have been using them in the mouth for more than 40 years. This video will be helpful for you to understand the difference between ceramic/zirconia implants and regular titanium implants.
I had implants put in place of 2 molars the dentist used 2 studs per tooth . 2 years ago I had pain and infection in booth of them . I went back and he xray them , xrays showed bone loss between studs . Now they feel loose and I can feel pressure when eating .. I brush day and use water pik for flossing .. what else can I do ? I’m scared that this was a waste of 9,000.00…
You need to be evaluated for the potential of a salvage procedure to graft back the lost bone versus explanting the implants.
Hi Dr Amin
I had a sinus augmentation done about 10 months ago, for my upper jaw. I sent you the scan. Please look at it. 2 dentist says just leave it alone , I don’t want to lose the bone added? Please advise .!thanks Susan
Hi Susan, you have been in contact with my office before but never scheduled the virtual consult. I wish I could look at everyone’s scans but that would be impossible has I receive hundreds of requests. You are welcome to come see me in person . I am certain I can fix your situation the first time.
😉
Thank you for your article. I ended up here because I have been going back and forth between my dentist/ periodontist and was beginning to doubt their ability to effectively diagnose me. This article confirmed a lot of the theories they have told me about why I may be experiencing this.
I have an implant on #9 that I got when I was 15. 10 years later, we found an infection that we believe was causing bone loss. I saw a periodontist who performed a surgery to open my gum line and clean the area.
2 years after this surgery, I have began experiencing the dull ache you mentioned. I have met with my dentist about it and he confirmed that my infection is back. He compared xrays from six months ago with today’s to confirm there is bone loss. I have always been worried about the noticeable recession on my gums in the front. I have also had this “bluish purplish” coloration for as long as I can remember. It looks like I may get a bone graft this time.
Diagnosis: I would appreciate any advice you have on keeping my dentist and periodontist accountable. What are some ways I can confirm bone loss is significant enough for surgery? Should I get a CT scan prior? What questions should I be asking during this process and during bone grafting process if we decide to do surgery? What are some ways that I can confirm my periodontist is experienced and competent for this surgery?
Maintenance: My dentist suggested better hygiene may curb this in the future, i.e. using a waterpik. Do you have any other advice for prevention? I am concerned about the long term affects of this as I am only 26 and want to keep this implant healthy long term. I am fearful of getting a bone graft and having this infection come back, eat away at the new bone, or damaging the tissue around the implant permanently. Will gum tissue grow back if I have a successful bone graft?
Lastly, do you have any additional thoughts about why this infection could have become an issue after 10 years? My dentist seems to think that because the implant was set when I was so young, my implant has recessed and created a deeper gum pocket, which is more prone to infection.
There are so many questions here I do not think I answered them all. I do suggest you get a 3-D scan before doing anything I’m surprised you have not had one already. This will allow the surgeon to evaluate and diagnose whether or not a salvage procedure is recommended or the implant should be removed. Removal and replacement is by far the most predictable option as opposed to salvaging an implant that has peri-implantitis.
Without seeing you I do not know why this has occurred. Sometimes there are simple answers and sometimes it just happens.
The gum tissue will not grow back in most cases
It sounds like you are pretty young and the first place to have an implant at age 15. He did not specify where this implant is in your mouth but if it is a front tooth this is very complex. You also have to evaluate the adjacent teeth to make sure they have not become affected by the bone loss..
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Hi I been to several periodontists as I have bone loss and need 14 pulled out. One says I should have pulled with bone graft put in at that time then later on have sinus lift and implant. Another which appears to be more skilled says to immediately have sinus lift , very large Implant installed and grafting done all at once. There is a lot of bone loss on on tongue side but plenty of bone on cheek side hence the reason the one thinks implant will work well… Others won’t even attempt the procedure… But I see the advantage of the one day procedure over multiple visits and higher cost of the conservative approach…. What is your take on all this…would a large I plant fuze all the bone back and make a good connection with the bone on cheekside.
tough call….that area can be tricky since the bone is so soft. Check out this post on internal sinus lifting..it might help you understand your options. I would have to see you to make a real answer.
Dr. Amin, Could you please recommend the best resource I can use to find a skilled and experienced doctor in the Boston, MA area to have implant work performed? Better yet, if you might have specific recommendations, it would be extremely helpful. I have both receding gums and some bone loss as well, so I need to find a practice which can address all of that.
I have tried to “Google” this, but am totally overwhelmed with the number of doctors that get shown in the search. I really don’t know where to begin.
Thank you.
AMERICAN academy of implant dentistry.
n preparation for my upcoming failed implant assessment which is now scheduled for September, my dentist, following periodontist’s instructions, took out the crown for #19.
My failing implant is #18. I don’t understand why the different tooth. Is this the procedure to prepare for bone grafting?
Please reassure me that all this is correct.
this is often a very good technique if the crown that was taken off is also an implant. This will allow the gums to cover over both of the implants and allow the surgery to be completed by having more gum tissue to suture together at the end rather than having open holes. Is this case?
this is often a very good technique if the crown that was taken off is also an implant. This will allow the gums to cover over both of the implants and allow the surgery to be completed by having more gum tissue to suture together at the end rather than having open holes. Is this the case?
If this is happening could it be the fault of the dentist I had implants put in and on the bottom a hole or space was left open and this is the area where I’m having reoccurring infections should I go to the dental office that did the procedure?
Peri-implantitis happens for so many reasons. There are times that it does occur due to poor implant position but it is so multifactorial it is hard to pin it down often. medical issues, bone anatomy, implant design, oral bacteria, and bite force, smoking, tissue thickness and about 100 other things all contribute
the link above talks about how to bone graft some of these cases. Good luck!
Thank you for this post it was extremely helpful. I am a 21 year old student who had an implant placed about a year ago i noticed some inflammation the last few weeks and went back to the dentist last week for him to tell me he was very concerned and I have lost a lot of bone due to plaque buildup? I explained that I brushed my teeth twice daily and that after having worn my retainer at night the inflammation got worse. He implied that not brushing my teeth was the cause as it ‘had to come from somewhere.’ I was quite disgusted as I take pride in looking at my teeth Im very upset and now looking at meeting with a gum specialist and have a second surgery as a student I dont know how I am suppose to afford all this? Is it worth getting a second opinion or do I have any other options?
Second opinion would be good.
implant dentist come in all ranges of skill, experience and judgment. Do you due diligence and try to find someone that can help you. Some peri-implantitis cases can be corrected with bone grafting very successfully. I hope this all works out for you.
I had an implant done on tooth #2, developed peri-implantitis and had surgery with bone grafting about a year to a year and a half later in September of 2016 Now I have it again and my periodontist recommended doing a second surgery. I’m a little hesitant since it did not work the first time but I also don’t want to lose the implant. Do you think it’s worthwhile to do the surgery a second time?
IF the prognosis is good then I would suggest doing. If this is a shot from half court, you may want to start over again
Hi I have had excessive saliva in my mouth like gunge, I had a full lower bridge implant March 2015, I went for check up two weeks ago and was told everything was fine, no X-rays were taken even though I said I had a funny taste in my mouth. I am very concerned as paid £12,000 + for my treatment.
Can you advise please
Thank you
Linda Grant
Extra saliva is always better than not enough. Have an X-ray taken to be sure.
Thank you for your reply, I can’t get appointment till Wednesday and there is a horrible thick gooey stuff in my mouth, I think it’s coming from my gums, it’s making me feel sick and high temperature, is this poisoning my system? I am am so afraid as it’s only Monday.
I have taken some antibiotics in the meantime.
Linda
I had 5 implants placed in the mandible all in the chin area due to not enough bone in the jaw. The original treatment plan was 4 implants but in this case a 5th implant was placed. 3 months later the surgeon checked the implants to see how they had integrated. They were fine but one had threads showing and the surgeon said that he could see plaque on the threads under the gum tissue. He said that bone loss was present (that is why the threads were showing) and would progress. The bone loss seems to be toward the back on the tongue side or perhaps between the implant on the one next to it. It’s hard to see because I’m wearing a temporary fixed prosthesis. (I had pain and a lot of issues in this area from the very beginning) He told me the reason this happened is that I did not keep the area clean enough. I doubt this is the reason, at least not 100% as I did everything I was told to do and more. How quickly does this bone loss progress in this situation? There is no pain, no swelling, no infection, at this time. Long story but the surgeon who placed it is not going to be taking it out. The implant is Nobel active regular size implant. This implant is on the end, I think #29? it is critical to the success of the treatment plan and placing a non removable prosthesis
I would take it out and replace it right away. If it is the terminal and of a fixed lower bridge such as a Prettau dental implant bridge, it needs to be solid. You only encounter problems 1 to 5 years later if it is left alone. Oral hygiene can play a part but it is not the only reason it implant can begin to lose bone early. Bone loss around dental implants tends to be progressive especially if it is on the outer wall. I know this is not what you wanted to hear but I would rather give you solid and truthful information that you can use.
The very problem you describe is exactly why I place all implants in a unique position much closer to the time in order to have the thickest bone possible on the outer wall and have it be stable for the next 20 years. It is possible that this was just a thin bone area and there is no option to place it closer to the tongue.
I like your analysis of bone loss which I have had since the eighties.
3 implants in the upper right quadrant hair place by Mexico dentist in 2000 I believe.
Now I have at least one that is loose and I think I’d like to glue it however I know the importance of bones and teeth and stuff.
Have an appointment the 25th of January at West River periodontics and I believe this guy is a problem solver will see!
Thank you for sharing your knowledge.
Can peri-implantits cause any sort of health concerns anywhere other than the teeth that is implanted?
You would have to be unusually severe and on more than just one tooth to cause an infection beyond the area of the teeth. If you have a compromised immune system it could spread something faster but typically the health concerns are limited to the mouth but inflammation anywhere in the body is not good for you.
One of my dental implants, placed in May 2016, has significant bone loss around the implant. The plan is to remove it, clean it thoroughly, more bone grafting and try the implant process again. My concern is whether this is a matter of malpractice or bad luck. I didn’t have any symptoms until two months after the placement of the crowns which I can’t help but wonder if my dentist did something improperly? I might add I am only 21 years old with no health conditions (to my knowledge) contributing to the bone loss.
It happens to the best of dentists and the best of patients. Just make sure your DDS is very experienced and of course have a scan before placement.
I would suggest you wait six months before you place the second implant.
Hi..I have had 2 dental implants , lower right, 1 which is now infected, taking Clindimycin since 10/11, was advised to try to save the implant even thought ex rays show 50% bone loss..My surgeon says I’m in the grey area..I’m considering removing it. I’m really torn because it’s so expensive , and if bone grafting doesn’t take then I have to add the expense of removing it. and choose to do a bridge with a supported implant on one end and natural tooth with Crown molar, which is rather short
.Don’t know if the supporting teeth will support the bridge as I have strong bite..Lots of anxiety over what to do.
If you’ve lost 50% of the surrounding bone in a 360° direction then your best removing the implant. No one on this planet can rebuild bone 360° around the implant that has 50% loss
I know that is not what you want to hear but believe me this is a better choice.
Hi. I think I am having a dental implant emergency during this pandemic and am afraid dentists might be closed. My 18 year old implant is getting looser and sorer every day… front tooth done by Dr. Don Kobashigawa and Dr. Steven Exler. But now I am 54 and a cancer survivor so my Arimidex is causing osteopenia and I think I am having bone loss and I fear an infection is around the corner. Can you help me?
It sounds like the implant needs to come out. The office is currently closed due to the COVID 19 virus pandemic. In order for dentistry to do its part to mitigate the spread of COVID-19, the Centers for Disease Control, CDA and ADA has mandated dentists nationwide to postpone non-emergency dental procedures for the next 2-4 weeks (maybe longer.) My hands are tied! We stand behind our governing associations and agree this is the “right thing to do.” We are also trying to save personal protective equipment for our medical colleagues who are more in need.
In the meantime, just keep it really clean. I would suggest a waterpik asap.
Stay safe. We will get through this.
Tooth #8 – I had bone graft surgery and implant surgery in April 10, 2015 and implant 11/13/15. On May 9, 2016, the crown was cemented in by another dentist. By June 8th, I had an abscess. I visited both the surgeon and the restoration dentist on that day. The surgeon declared it wasn’t the implant and the dentist cleaned the tissue and I returned on 6/13, 6/29, and, 7/6. I was advised to return to the surgeon at the 7/6 appt. On 7/7/16, I saw the surgeon. He cleaned up the gum and said no anti-biotics were needed. I returned 7/12 and on 7/15, the surgeon backed out the abutment just a little. By this time the crown was broken off and removed by the dentist. Reversing the abutment began the healing process.
On 9/14, after a re-check the dentist re-installed the temporary. When I was leaving, I mentioned the tooth felt like it moved a little. As it turns out, I had to return on 9/15 (next day) because the abutment was loose.
On 10/3/16, I returned t the dentist for a new temporary so we could see how the tissue reacted. The next day, I bit into something with the tooth next to it and heard a loud snap. October 4th, back to the dentist. I broke the screw on the temporary. He then set the permanent tooth in place but did not cement it because the color needed one more tweak.
I visited the lab on 10/6 and left with the crown. On 10/7 I returned to the dentist and he cemented the crown in place.
Today is Monday, 10/10/16 and the tissue has begun to ache and it looks darker. It is becoming more tender when I touch above my lip. At this juncture, I do not know whom to visit. From what I have read now that I am researching this, I am guessing I should have a 3D x-ray.
If you have any intuition as to what may be happening I welcome advice. After the first crown was removed, the tissue healed and the only thing irritating it was the temporary crown movement. I live in the northern suburbs of IL, Crystal Lake.
Very odd. I think the implant is failing or the abutment is loose. Both are uncomfortable and uncommon. Get a pa xray and a 3D ASAP.
6 implants on upper jaw with a hybrid one piece fixed bridge. One implant upper left quad has severe bone loss after 15 years. Can I have another hybrid made and use the 5 implants that don’t have bone loss and remove the bad implant. Looking for least expensive option. I’m not working right now.
This is exactly why I do not suggest the all on 4 procedure were only 4 implants are used to support an entire bridge. Your situation permanently describes how you can remove one dental implant and typically continue to use the same bridge or modified. If you’re existing 5 implants are solid by all means try to make a new bridge just using the 5 of them or modify your existing.
Hi there,
Aug 2012 I had a root canal extracted, synthetic bone build up and implant put in behind my canine tooth (top left side).
The implant is between 2 root canaled teeth.
It healed good. Then I had the tooth put on the implant Feb 2013.
I started getting a bad metallic taste in my mouth. It was constant. Feels like something sloughing in my mouth.
I went to the surgeon twice
about the taste/sloughing but after taking a 2d image said it looked fine and blamed it on nerve pain.
After 1 year I had the tooth removed from implant.
Hoping the taste would go away but it did not.
Taste is still there .
Sept 2016 I saw another surgeon about a tooth behind the implant.
He took a 3D X-ray.
He said that 1/2 the bone if fine but 1/2 of the bone on the other side is gone.
Why would this happen?
What are my options?
Can you give me any advise or recommendation?
I have been tasting this for about 3-4 years. Could I be tasting the bone sloughing ?
I taste metallic, blood and burntness that is getting worse all the time.
I appreciate any advise you can give me.
Thanks
Christine
We don’t know why on 100% of all cases. And my practice about 1% of patients will develop this condition. You may want to cut your losses and remove the implant and start all over again. I know you don’t want to hear that but often it is the best advice. 50% bone loss is extreme. It needs to be removed ASAP.
My mother has peri-implantitis. Her dentist told her to go to an oral surgeon to have all of her implants removed, because the inflammation and infection is so bad. She doesn’t want to have surgery so she is refusing to go to the oral surgeon. What could happen if she continues to refuse to get them removed ?
Thank you for your help!
Continued bone loss and chronic long term low grade infection. So sad…..all of them???? That is so rare.
Her bone may be the type that just dissolves over time.
I had two failed bicon implants, teeth #4 & #5. I have endured unbelievable pain even now after second one was surgically removed. The first was removed by hand, no instrument required. Now months have passed and some days I continue to have incredible pain from the site. The bone loss has continued and I am greatly concerned as to if and when the bone loss and pain will ever stop. According to the second dentist who removed the implant, the initial implants were not properly placed. The implant he removed was infected as well as the first. I also explained to the initial dentist I’d been diagnosed with osteoporosis and he said that should not be an issue. I now have a partial I seldom wear. Please advise. Where are you located? Thank you!
are you sure it is not another tooth like tooth #3 or tooth #7?????…. Believe it or not, this happens more often than you think where pain is coming from an adjacent tooth and the patient does not even know it. I am located in Burbank California.
This is very odd and I can see how it is troubling you!!
Paid DR. Xxx. Xxxxx of Englewood N.J. $29,000.00 for my dental implants, they were not proper placed, the uper denture rocked in my mouth had a bar across the top of implants bar broke snap on denture after 5 mouths the clips wore out, made of plastic, he tried different clips ,still got loose,he was not explaining why , his receptionist Heather told me to look for new dentist .
She told me if in any pain they will give me medication for 30 days ,I can no longer be his patient ,after 10 yrs a 93 yrs old dentist told me the answer ,it rocks ,I had front teeth on the bottom, minus a total of 4 back teeth Dr. Matriess said ,I had no foundation, can’t build a house with a full foundation.
I had an unsuccessful dental implant that originally took, I also had grafting, then the bone around it desinigerated. What could be some reasons for that? Might another be successful? I also heard that being on an antidepressant or other RXs might affect the implant! Are there prescriptions that might be a factor in the loss?
All of the things you have said so far are correct. Yes some antidepressant medications are known to have negative effects on dental implants.
Another implant will likely work even though the first did not. Often times bone is lost for no reason at all but often there are significant medical or dental issues that have caused it.
Hi Dr Ramsey
I wish you were in Houston:) I had all on 4 about 3 yrs ago I think I have 2 implants in front trying to fail!!! I have lost a lot of bone . I’m on my second set of teeth 26000.00later and still not done!!!! Looking at possible grafting next!!!!
Ugh. This is why I strongly suggest against the all on four. There is no “back door” to escape…no spare tire….you have to throw away the whole car.
I recently had one implant not take on an upper “all on 8”. The solution was just to remove it and now it is still a strong “all on 7”.
The solution is to unfortunately start over but please design it with minimum six implants for the upper and make sure there is thick bone on the outside of all implant. This is the only way this is going to last.
I have minor peri implantitis at one of multiple implants. My dentist sent me to a periodontist who wants to do gum grafting around the implant. The only issue I am having is sensitivity when I floss and water pik. Is this a recommended procedure?
If you are losing bone, it is often progressive leading to the loss of the implant. Generally a 3-D scan would be suggested to evaluate the position of the bone loss. I would suggest you do this before any type of rescue procedure.
I had a dental implant a few years ago and on my recent 6 month cleaning/X-rays, a new dentist (we moved states) noticed I had bone loss in the area. He questioned the length of screw used. My formEr dentist did prep work, been with practice for 13 yrs, felt confident in their work and referral of endodist who performed procedure. My current dentist suggested a low level laser to regenerate bone(I had no pain prior to this) which will be 3 weeks tomorrow I had it done. I still feel pain and having to take at least 8 Advil a day. Called back after first week of having procedure done & they took X-ray, said everything looked good, still experiencing pain after 2nd wk, told to give it another week and I still have dull ache today. Is this normal or is X-ray not showing an infection, something is going on. I even took norco prescription (3 days and didn’t have much relief. Thanks for any insight you can give me. Questioning this new dentist????
low level laser treatment may reduce the pocket but will not likely regenerate bone. Peri-implantitis is difficult to treat without surgically opened in the area and doing a bone graft/smoothing threads off of the implant/cleaning all the inflamed tissue out. It is not normal to have pain this long. I would go back and have another follow-up visit.
I want to share one case of implant placed in maxillary premolar region in 45 yes female….I HV xray record pl send me your email I’d so I can share xrays
That implant has lost a tremendous amount of bone. You would be much better off removing it entirely and starting over. It will be forever compromised should you decide to keep it.
Ramsey Amin DDS
I had a dental implant done on tooth #10 January 22, 2015. I learned in October via Xray that I have none loss. The periodontist says the implant is stable. However, I have 3 threads exposed. No other symptoms. However he says I need to wait another 3 months because it has not been a year for the osteointegration needs the full year. Then he will reexamine and will plan for a debridement and procedure for bone grafts. Do you agree that we need to wait the 3 months?
1 year is a good milestone before attempting intervention on a new implant as long as it is not progressing quickly.
I have major problem with implant bone loss due to bone grafting, and I would like to come for consultation at your office. Do you charge for consultation or is it free.
Please let me know so I can schedule an appointment.
Thank You.
Hi Lina,
I would be happy to help you personally. The best thing for you to do would be to call and speak to one of my front office receptionists. They are highly skilled and would be able to answer all of your questions. There is a charge for the initial consultation.
Office phone number: 818-846-3203
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
My Hygienist has me using Perio Gel on on molded plastic trays 4 times a day for 15 minutes everyday. Is this another method to treat implantitis?
It may buy you time depending on the condition and the extent of the peri-implantitis. If the threads are exposed and a 360° pattern, there will be fewer options for successful procedures. If you have a one-sided bone defect, that may be able to be grafted.
Good luck,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
I had a Prettau cement retained full lower bridge using 6 implants. placed in Feb. 2015 and a separate implant and zirconia crown on tooth #19 at the same time. I complained about minor pain at the time, and it continued. Went back a month ago. They didn’t see anything with an Xray and cleaned the bridge. Two weeks ago I started to experience real pain all around that implant with no let up . I am going back on Monday,But I decided to do my own research as I have all during the process over 3 years. and now I think I am facing what you describe in you article. I won’t hesitate to have the implant removed, because I don’t need it. Prior to the implants I lived with with a cantilevered bridge hanging on 4 teeth with crowns. all the way to tooth 18 for 28 years. . There is no pain at implant 18 so I can hope the bridge and bone will survive. But I won’t be surprised to hear them say the best thing is to remove the implant. Sound about right???
If it is deemed that the implant has so much bone loss that cannot be corrected, the best option is to remove the implant like you said.
Peri-implantitis can affect a few implants. My guess is your bone and/or gum is very thin in that area which is a risk factor for developing peri-implantitis.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
I have 5 teeth in front at the bottom and 6 teeth in front at top. Then I have one 3 tooth bridge and a tooth on my bottom right. Rest are all gone. I am wondering if I should get all implants or 3 implant bridges- for top left, bottom left, and top right jaw? Or something else. These implant bridges will be on replacing the chewing areas; will they be stable?
Hello Ronnie,
I do not have enough information about the 5 teeth in the front at the bottom and the 6 teeth in the front at the top. Obviously I would need to see x-rays and 3-D scans in order to steer you in the right direction. Oftentimes the remaining front teeth are the last wants to go but have significant bone loss or not strategically favorable for reconstructing the whole mouth.
The decision to make 3 segmented Bridges versus a one-piece is very unique to each person. Segmentation is always nice because it allows you to maintain the most natural feeling teeth possible. That being said a requires more implants and more bone to be able to do this.
Whenever you decide to do dental implants are extremely stable when placed correctly and when the teeth are made correctly. Hopefully you get 20 years out of them.
I believe on another post you asked if I could personally review your scans and do a consult with you because you do not live in the area. Call my office if this is something you would like to arrange.
Respectfully,
Ramsey Amin DDS
Hi, I am missing one top molar on each side. I never wore braces but did wear a retainer when I was about 17 to close the gap in my front teeth. Before losing molars about 20 years ago, I had pretty straight and nice teeth. About 1/2 a year ago I noticed my gap slowly opening n I hate it. Could I get a retainer to close again? Would I have to replace missing molars to get braces like Invisalign? Please let me know what my options are to close gap. At this point I feel too much time has passed to replace molars since it was 20 years ago and am sure of the bone loss. I am 44 yrs old.
More depressed every day.
Hello Norma,
Because the top molars have been missing for so long, you will likely need some type of sinus bone grafting. This can be a simple as an internal sinus lift or you may possibly require a lateral window sinus bone graft. Both of these procedures are extremely predictable and normal procedures that I perform multiple times a week. They are not rare or experimental.
There is no way for me to be able to completely tell you whether the gap can be closed with braces alone. You would need to see a dentist for a complete evaluation with x-rays.
Sinus Lift Bone Graft
Very Respectfully,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
I have recently been told that I can not have implants due to bone loss. I still have all my teeth, but it’s getting worse. Can the bone graft procedure be done in my case.
Hello Rudy,
Keep in mind that bone grafting can be done to rebuild most situations. There are times though where bone grafting will not work and other alternatives such as a bridge may become a better option. there are many different techniques of bone grafting and it will be highly dependent on your unique situation. In almost every situation I can rebuild bone to have implants. Sometimes if the implant is in the very front of the mouth on the upper and bone is missing on the palate, then there are issues building bone vertically.
I Don’t Have Enough Bone For Dental Implants
respectfully,
Ramsey Amin DDS
I had this problem and I ended up losing the implant. I wish I would’ve gone to a more experienced dentist. I went to one of those radial advertisement places… What joked it was. I should’ve gone with my gut feeling….now I need a pretty massive bone grafts in order to have another implant. The dentist that I saw said the implant was put in so deep in so far to the outside that it was going to lose bone no matter what.
Hi Sonia,
Sorry to hear about your mess. I have seen this too many times. There is no doubt that experience counts. Make sure you see a really expert provider to replace the implant a second time. Most dental implants last somewhere from 15-30 years.
Sometimes peri-implantitis cannot be avoided and is unknown, but it sounds like you and your case there was issues with the position of the implant.
The angle of the implant is really important.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry